Podcast: PHI’s Faces for the Future on How Investing in Youth Can Transform the Healthcare System
FACES Co-Founder and Director Dr. Tomás Magaña, along with alumnae Vanessa and Veronica, join the HHREC podcast to discuss how the program impacted their careers, aspirations and futures. The Faces program supports young people from low-income communities and communities of color to have the support, skills and confidence necessary to pursue careers in public health, medicine and related fields.
Since completing the program, Vanessa and Veronica have both gone on to become leaders in the field, now working at community health organizations as health equity experts and advocates. Their stories demonstrate how FACES is building long-term a pathway that helps to remedy the lack of diversity in health care professions, address health disparities and provide support, encouragement and connections for participants to launch sustaining, rewarding health and medical careers.
Watch the full episode, below:

I remember all the folks I shadowed at each of my externships. I remember them being people of color in the hospital, and I always thought that was so cool because I hadn't seen it before. To be able to have those mentors and safe spaces, to see someone who looks like you and can express a shared lived experience was very important.Vanessa
FACES alum

The good thing about learning those [mental health] skills [as part of the FACES program] is that we can bring it to the young people that we serve at our clinics right now.Veronica
FACES alum
FACES works in partnership with schools, healthcare systems, local organizations and communities across the country by incorporating best practices in youth development, stakeholder engagement and workforce development strategies. FACES Co-Founder and Director Dr. Tomás A. Magaña also discusses the program’s approach to providing a cohesive system of support for youth to ensure highly qualified, multi-lingual and multi-cultural health care professionals who are able to meet the growing demand of the workforce.
Through a comprehensive investment in young people, we can ultimately transform healthcare, and the way it is practiced—both by diversifying the workforce so that it better reflects the communities we serve, but also by bringing the skills, the talents, the power, the agency of our young people.Dr. Tomás A. Magaña
FACES Co-Founder and Director
Video Series: Understanding Telehealth
The Telehealth Learning Series from PHI’s Center for Connected Health Policy is designed to provide a deeper understanding of what telehealth policy is and how it affects us.
Navigating the telehealth policy landscape can oftentimes feel overwhelming and quite complicated. This Telehealth Learning Series from PHI’s Center for Connected Health Policy (CCHP) is designed to help provide a deeper understanding of what telehealth policy is and how it affects us.
In this first informational video of 2024, CCHP Executive Director Mei Kwong delves into the intricate landscape of US telehealth policy, offering insights into the latest developments shaping the future of healthcare delivery. Topics addressed in the video include: An overview of the federal and state telehealth policy landscape; the current status of certain policies, such as those related to Medicare and prescribing controlled substances; and items to monitor over the coming year, such as Artificial Intelligence (AI) and cross-state licensure.
Watch the Telehealth 301 playlist
Telehealth 301 – Medicare’s 2022 Telehealth Policies on Mental Health
This video offers a deep dive into the different telehealth policies related to mental health that went into effect in 2022.
Telehealth 301 – How Court Cases Make Telehealth Policy
CCHP’s executive director, Mei Kwong, provides insight on how court cases can also develop telehealth policy.
View the Telehealth 201 playlist
Telehealth 201 – Medicare Telehealth Coverage
In this short video CCHP’s executive director, Mei Kwong, provides a primer on how Medicare policy gets created, who can act to make change and the difference between “telehealth” and “communications technology based services (CTBS)”.
Telehealth 201 – Medicaid Telehealth Policy
In this short video CCHP’s executive director, Mei Kwong, provides a primer on Medicaid and telehealth policy.
Telehealth 201 – Licensure
In this short video CCHP’s executive director, Mei Kwong, discusses licensure as it pertains to telehealth.
Telehealth 201 – Prescribing
In this short video CCHP’s executive director, Mei Kwong, provides a primer on telehealth prescribing policy.
Telehealth 201 – HIPAA & Privacy
In this short video CCHP’s executive director, Mei Kwong, discusses how telehealth works with HIPAA and health privacy laws.
Catch up on the Telehealth 101 Series launched fall 2021
Telehealth 101 – What Is Telehealth Policy?
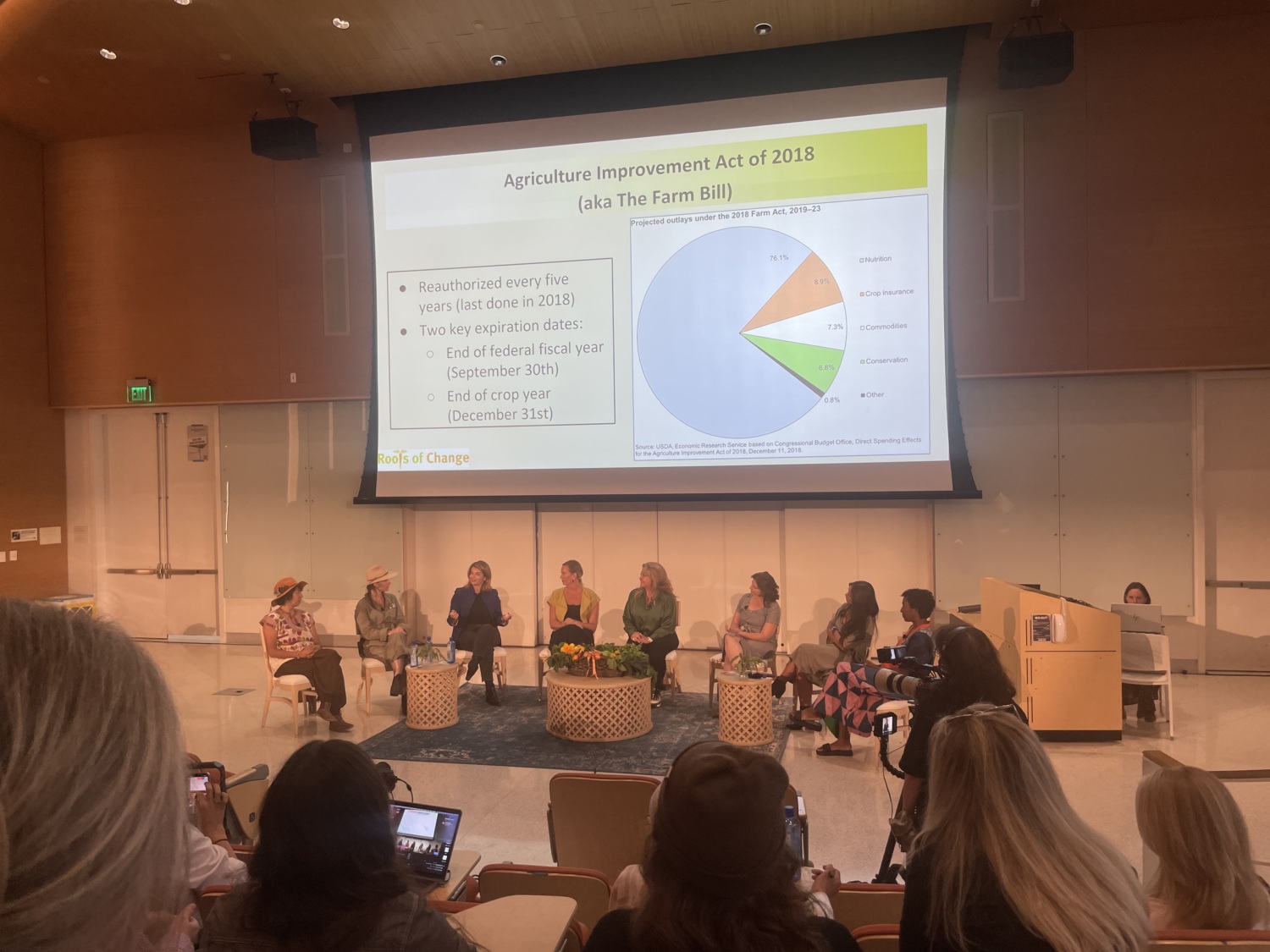
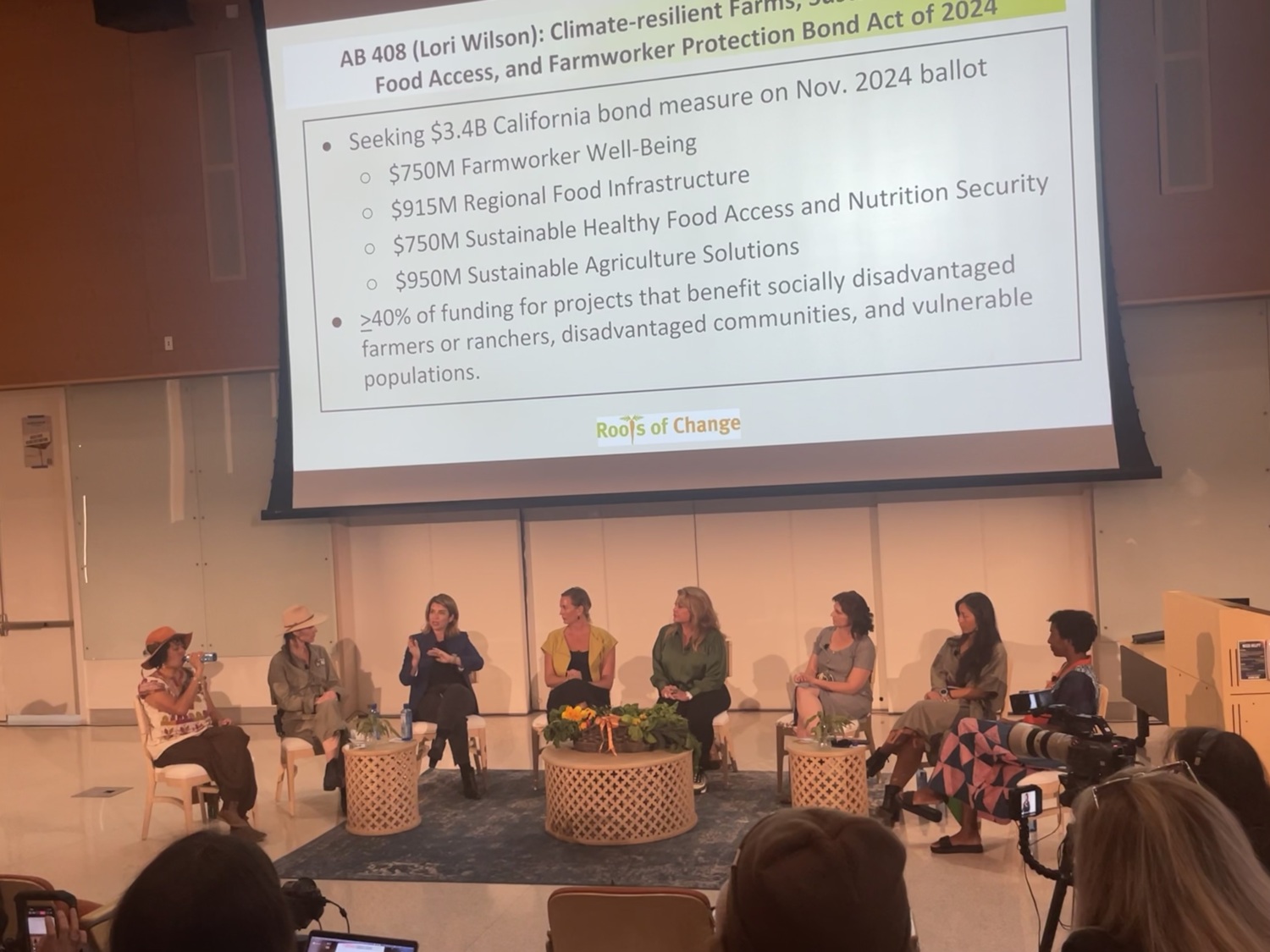
Generation Regeneration: Women Forging Change (Future Thought Leaders Panel)
Lesley Kroupa, policy specialist at PHI’s Roots of Change and PHI’s Center for Wellness and Nutrition, joins a panel of experts to discuss how to make nutritious food accessible to all without depleting the earth.
In December 2023, the Berry Good Food Foundation held its 12th Future Thought Leaders Panel: Generation Regeneration: Women Forging Change, featuring women farmers, winemakers and community builders at the forefront of the regenerative food movement. The discussion covered conservation, biodiversity, soil health, carbon reduction and more—all which can ultimately lead to a healthier food system, food security and a balanced economy for generations to come.
PHI’s Lesley Kroupa was a featured panel guest who joined other experts to discuss how to make nutritious food accessible to all without depleting the earth. Lesley is a policy specialist at PHI’s Roots of Change and PHI’s Center for Wellness and Nutrition working to ensure emergence of a sustainable food system in California. See the recording below:

Our work at Roots of Change at the Public Health Institute is about listening. Listening to all these experts who have their hands in the ground telling us, “Hey you know what we need help with, please elevate our voices in this way,”... [because] so many of our policies at the state and federal level are counterproductive to [their needs].Lesley Kroupa
Policy specialist at PHI’s Roots of Change and PHI’s Center for Wellness and Nutrition
The panel also featured other women in the regenerative food movement, including Michelle Ciccarelli Lerach, founder of the Berry Good Food Foundation; Bea Alvarez, climate resilience specialist at FoodShed Small Farm Coop; Lily Foster, founder of Fenix Farms; Kristin Magnussen, winemaker at Lechuza Vineyards; Elle Mari, director, Urban Food Equity, UC San Diego Center for Community Health; Keiko Nishikawa, winemaker at Santo Tomas Vineyard; and Mia Vaughnes, founder of Good Neighbor Garden.
Webinar Recording: Racism, Housing and Asthma
In December 2023, PHI’s Regional Asthma Management & Prevention (RAMP) and the National Center for Healthy Housing (NCHH) jointly hosted a conversation on the connections between racism, housing and asthma with three of the country’s leading practitioners and researchers in this space:
- Tyra Bryant-Stephens, MD, Children’s Hospital of Philadelphia
- Neeta Thakur, MD, MPH, University of California San Francisco
- Adali Martinez, MD, MPH, University of California San Francisco
Among those providing asthma home visiting services and/or working toward scaling and sustaining asthma home visiting services, many agree that housing is one of the most critical social determinants of asthma health disparities.
Further, we know that poor housing conditions are not the result of individual behaviors nor happenstance. Rather, poor housing conditions in BIPOC communities are a direct result of historical and current policies and practices imbued with structural racism, including redlining, industrial zoning, exclusionary zoning, discriminatory or predatory lending, and systematic displacement.
With this shared recognition, it’s important to explicitly name and address structural racism. Each of the three conversation participants are doing this through their work and their research. Through this conversation, they challenged and motivated those working across the spectrum of activities to improve asthma outcomes to take action with a long-term vision of racial equity.
Additional Resources
Presenters
- Dr. Tyra Bryant-Stephens is a board-certified pediatrician in clinical primary care practice for over 35 years and Associate Professor of Pediatrics at the Children’s Hospital of Philadelphia. In 1997 she founded the Community Asthma Prevention Program (CAPP) of Children’s Hospital of Philadelphia (CHOP), an asthma program that implements asthma interventions in underserved, under-resourced inner-city communities. When CHOP launched its Center for Health Equity in 2021, Dr. Bryant-Stephens was chosen to lead the Center and now serves as AVP, Chief Health Equity Officer. Dr. Bryant-Stephens is nationally recognized for her work in community-driven, evidence-based research in asthma interventions. She served as a member of the Expert Panel Working Group of the National Heart, Lung and Blood Institute which released the 2020 Focused Updates to the Asthma Management Guidelines. She currently serves on the federal advisory asthma committee, National Asthma Education and Prevention Program Coordinating Committee (NAEPPCC).
- Dr. Neeta Thakur is an Associate Professor and the co-Director of the Partnerships for Research in Implementation Science for Equity (PRISE) Center at the University of California, San Francisco (UCSF). Over the past decade, Dr. Thakur has developed a novel research agenda that is directed towards 1) defining obstructive lung disease phenotypes that exist in racially and ethnically diverse communities and how these are shaped by social and environmental stressors, 2) identifying community-specific drivers that place individuals at high risk for poor outcomes, and 3) co-developing place-based and targeted interventions aimed at social and environmental stressors to improve respiratory outcomes in historically marginalized populations. Over the last five years, she has served on several expert panels, including the EPA Clean Air Scientific Advisory Committee PM Panel and the NHLBI National Asthma Education and Prevention Program Coordinating Committee.
- Dr. Adali Martinez is a second year pulmonary & critical care fellow at University of California San Francisco where she also completed her residency and chief residency. As a chief resident, Adali played an integral role in building upon UCSF’s existing Diversity, Equity and Inclusion curriculum to include programming to guide trainees on incorporating the principles of antiracism in medical education, clinical practice and research. Her background prior to her medical training was in health policy and advocacy at the local and state level. Under the mentorship of Dr. Neeta Thakur, her research focuses on addressing the impact of chronic stress and environmental exposures on asthma outcomes.
- Moderator: Amanda Reddy, MS, is the Executive Director of the National Center for Healthy Housing, an organization founded on the premise that better housing can be a powerful platform for better health. Amanda describes her path into the field of environmental health by saying that she took a job and found a calling. Over the last 15 years, she has answered that call by working with communities to effectively prevent housing-related illness and injury by implementing evidence-based and equitable policies that improve housing quality. Prior to joining the National Center for Healthy Housing, Amanda was a research scientist with the New York State Department of Health, where she supported a range of programs focused on improving indoor and outdoor air quality in homes, schools, workplaces, and outdoor settings. Amanda has served as a national leader in securing sustainable financing for healthy homes services and developed a talent for making topics like healthcare financing, code enforcement, and economic evaluation engaging. She holds degrees in environmental health from the London School of Hygiene and Tropical Medicine and neuroscience from Mount Holyoke College.
Webinar Recordings: Racial Trauma Among Asian American & Asian Immigrant Communities
In this webinar series, PHI’s Lotus Project addresses the impact of AAAI hate, and how to better support AAAI communities. Catch up with the recordings.
Anti-Asian hate crimes have risen dramatically during the COVID-19 pandemic, with more than 11,400 hate incidents against Asian Americans reported to the national Stop Asian American and Asian Immigrant (AAAI) Hate coalition between March 2020 and March 2022. However, racism, prejudice, and acts of hate and violence towards AAAI communities have historically existed ever since members of these communities first began immigrating to the United States.
Racial stress and trauma can be caused by direct or indirect exposures to racism throughout one’s lifetime and is influenced by an accumulation of unavoidable exposures to racism across generations, communities, and history. The impact can negatively affect the mental health of many generations.
In 2023, PHI’s Lotus Project hosted a webinar series to educate on the impacts of AAAI hate and explore how to better support AAAI communities. See the recordings:
Webinar 1: Historical Context & Mental Health Impacts (2/1/2023)
This webinar and panel discussion explores the historical context of AAAI hate, its connection to current events, as well as the impact of AAAI hate and racial trauma on the mental health of youth and families. Participants learned about key concepts related to the history of racism towards the AAAI community, such as the model minority myth, and the mental health impacts of racism and trauma on AAAI children, youth, and families.
Webinar 2: Implications for Clinical Practice (4/25/2023)
This webinar takes a deeper dive into culturally sensitive and trauma-informed clinical practices and recommendations that can be implemented to best support AAAI children, youth, and families who have experienced any form of racial discrimination, stress and trauma. Participants learned how to describe trauma and mental health issues in AAAI communities due to exposure to anti-Asian hate, particularly during the COVID-19 pandemic; and identify cultural sensitive clinical practices to support AAAI children, youth, and families.
Webinar 3: Community Programs in Action Recording & Slides (8/16/2023)
This webinar explores specific culturally competent and trauma-informed community-based programs that have been implemented to support AAAI children, youth, and families who have experienced any form of racial discrimination, stress and trauma. Participants learned how to describe at least two community-based programs that have been developed and implemented to address trauma, mental health issues, and impacts of anti-Asian hate in AAAI communities; and identify at least two strategies on how to implement culturally competent community-based practices to support AAAI children, youth, and families.

Resources on Addressing Anti-Asian American and Pacific Islander Hate
In collaboration with the National Child Traumatic Stress Network (NCTSN), forming the NCTSN AAPI Resource Collective, the Lotus Project developed and published two resources on historical trauma in AAPI communities and on having tough conversations about anti-AAPI hate with children.
Talking with Youth about Anti-Asian American and Pacific Islander Hate Resource
This AAPI and age-specific resource discusses how anti-AAPI hate can impact children and youth and how to best support and talk to them about anti-AAPI hate, race, and ethnicity.
Rise of Anti-Asian American and Pacific Islander Hate
This resource highlights the importance of acknowledging historical trauma and its impacts by providing a brief overview of key historical events that the AAPI community has experienced that continue to impact the community to this day.
The Lotus project aims to provide training, education, and technical assistance based on the wide-scale dissemination science and implementation of effective, evidence-based trauma-informed treatment and service approaches specific to Asian American and Asian immigrant (AAAI) populations. This work is a collaboration of two key agencies, PHI’s Health Intervention Projects for Underserved Populations and Richmond Area Multi-Services (RAMS).
Workshop Recordings: Supporting AAAI Communities in Healing from Racial Trauma
See recordings from the Lotus Project’s in-person workshop on how to better support AAAI children, youth, and families with healing from racial trauma and incidents of anti-Asian hate and discrimination.
Racial stress and trauma can be caused by direct or indirect exposures to racism throughout one’s lifetime and is influenced by an accumulation of unavoidable exposures to racism across generations, communities, and history. While anti-Asian hate crimes have risen dramatically during the COVID-19 pandemic, the experience of racial discrimination and violence is not new to Asian American and Asian Immigrant (AAAI) communities. The impact can negatively affect the mental health of many generations.
In May of 2023, PHI’s Lotus Project hosted an in-person workshop to explore how to better support AAAI children, youth, and families with healing from racial trauma and incidents of anti-Asian hate and discrimination. The Lotus Project is an initiative of PHI’s Health Intervention Projects for Underserved Populations.
Watch videos from the workshop:
- Welcome Note: Presented by Won-Fong Lau Johnson, PhD, NCSP
- Session 1: Yellow Peril Racism Past, Present and Future | Presented by Russell M. Jeung, Ph.D
- Session 2: Barriers to Mental Health Access in AAAI Communities
- Session 3: Culturally-Informed Clinical Practices for AAAI Mental Health
- Session 4: Building and Nurturing Healthy Community Alliances
Welcome Note: Presented by Won-Fong Lau Johnson, PhD, NCSP
Session 1: Yellow Peril Racism Past, Present and Future | Presented by Russell M. Jeung, Ph.D
Session 2: Barriers to Mental Health Access in AAAI Communities
Presentation 1: Barriers to Accessing Mental Health Services in the AAAI community: Youths and Families
Presented by Anne Lew, M.S., AMFT (See Slides)
Presentation 2: Addressing Medication Stigma and Limited Access to Culturally Competent Care in the AAPI Community
Presented by Michele Woo, Psy.D (See Slides)
Presentation 3: Vantage Point from a Community Based Organization Presented by Sonnara Sen, ASW (See Slides)
Panel Discussion Moderated by Angela Tang, MSW, LCSW
Session 3: Culturally-Informed Clinical Practices for AAAI Mental Health
Presentation 1: Supporting Asian American and Asian Immigrant Communities in Healing from Racial Trauma in Community Mental Health
Presented by Christina Yu, LCSW (See Slides)
Presentation 2: Cultural-informed Therapy for Complex Trauma in Asians/Asian Americans
Presented by Christine Chang, PhD (See Slides)
Session 4: Building and Nurturing Healthy Community Alliances
Event Photo Gallery
Really enjoyed all the presentations and learning about how the AAAI/AAPI community can work together to get through trauma & racial trauma.Workshop Attendee
(It was helpful) to learn new perspectives of other CBO’s outside of my community.Workshop Attendee
I enjoyed the variety of lectures and learned a lot from very engaging speakers.Workshop Attendee
Networking, resource sharing & applied examples (were the most helpful).Workshop Attendee
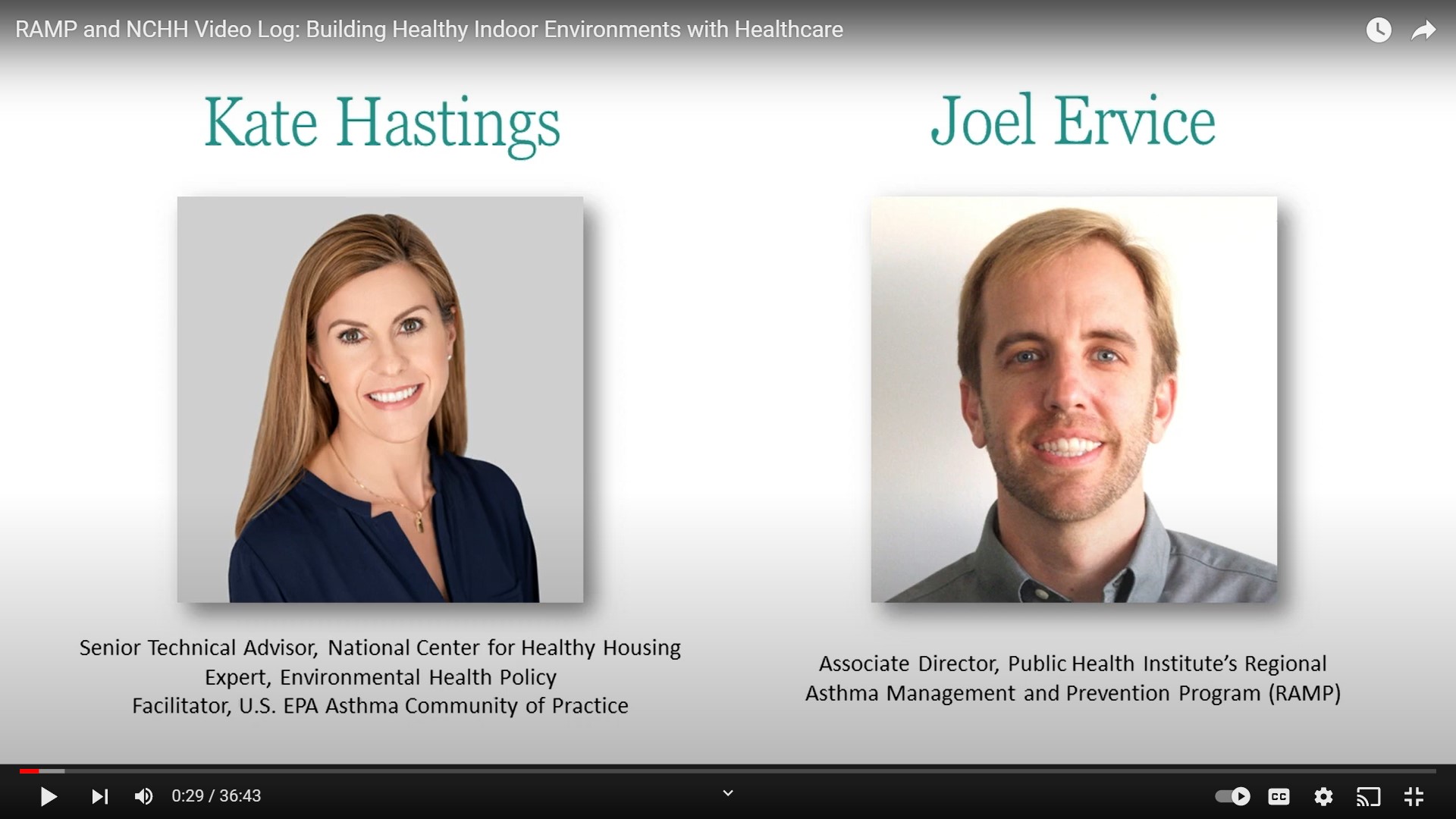
Video: Building Healthy Indoor Environments with Healthcare
PHI’s Regional Asthma Management Prevention’s (RAMP) Associate Director Joel Ervice interviews Kate Hastings with the National Center for Healthy Housing (NCHH) about how the healthcare sector can support healthy indoor environments.
The healthcare sector can play a critical role in improving the indoor environment for people with poorly controlled asthma. Policy wins in California and elsewhere underscore this important relationship. How can we build on initial advances across the country? How can we more effectively leverage partnerships and resources between healthcare and asthma and healthy housing stakeholders to help people most in need?
In this interview, Joel Ervice with PHI’s Regional Asthma Management and Prevention program and Kate Hastings with the National Center for Healthy Housing take a deep dive into health care policy focused on built environments as good health investments.

Healthcare is the largest and fastest-growing part of our U.S. economy, but it’s not providing a return on investment to our society. We spend more money on healthcare than any other developed country, yet we don't get better outcomes. The cost of healthcare in the United States is just growing. Chronic disease disparities are the largest part of our growing healthcare costs.Kate Hastings
Clinical healthcare knows that a lot of those chronic disease disparities originate and are made worse outside of the clinic… Healthcare partnerships around home environments are just a national imperative.
Senior Technical Advisor, National Center for Healthy Housing Expert, Environmental Health Policy Facilitator, U.S. EPA Asthma Community of Practice
PHI’s Regional Asthma Management & Prevention’s (RAMP) mission is to reduce the burden of asthma with a focus on health equity. Emphasizing both prevention and management, RAMP builds capacity, creates linkages, and mobilizes networks to advocate for policy and systems changes targeting the root causes of asthma disparities.
Webinar Recording: Better Data for More Equitable Public Health Research
In this webinar recording, PHI’s President and CEO Dr. Mary Pittman joins Research!America for a discussion about what good data really looks like in the context of public health research.
Research is only as good as the data informing it. In April 2022, PHI’s President and CEO Dr. Mary Pittman joined Research!America for an alliance discussion about what good data really looks like in the context of public health research.
In this discussion, Dr. Pittman explores tools and approaches to make data more precise, and how social determinants of health and other community-informed measures provide critical context to make public health data—and the research that comes from it—more meaningful and actionable.

Data is only as good as its applicability by our communities. Data is not neutral, and if we want to build health equity, we need to examine the scientific quality and quantity of the data we get—but also make sure that we are listening to communities to see and address what the data may be missing.Mary A. Pittman
PHI President and CEO
Learn more about how PHI uses data to shape equitable solutions:
- PHI’s Healthy Places Index (HPI) mapping tool: The HPI tool, developed by PHI’s Public Health Alliance of Southern California, is a powerful data, mapping, and policy platform designed to identify opportunities to improve neighborhood health in areas where it will have the strongest impact on life expectancy. Public health and health care leaders have used HPI to guide public health resources for years; during the pandemic, it became a core tool to guide COVID policy and strategy, particularly to identify and direct resources to communities experiencing the most disproportionate impacts of COVID-19. The HPI tool uses census tract data, to drill down to the neighborhood level, which reveals micro-level disparities–like families experiencing high levels of food insecurity–so we can develop tailored responses.
- PHI’s Research on Pregnant Women and Offspring Exposure to Toxic Chemicals: PHI’s Child Health Development Studies tested blood levels of 150 Black and 150 non-Black women for chemicals like pesticides. Instead of simply publishing their findings, they shared back the results, individually and as a cohort. The personal report-backs led to greater motivation to access health and safety information, and increased engagement with the reports among Black participants.
- Experts Weigh in on Chemicals in Bay Area Drinking Water: After California’s Paradise Fire, neighbors were concerned about home drinking water safety. PHI’s researchers tested water samples for chemicals, and provided results directly to the community—helping to mitigate some of the ongoing trauma and trauma from the wildfire and support rebuilding a sense of community and personal agency.
- PHI’s Study Reveals Inequities in Alcohol Screenings, Resulting In Missed Opportunities for Treatment: PHI’s Alcohol Research Group (ARG) examined the impact of Medicaid expansion on alcohol and opioid treatment admission rates among adults. Medicaid expansion led to increased Medicaid-insured alcohol and opioid treatment rates in the general population, and particularly among Black and Hispanic/Latinx groups. The study’s findings also suggest that there are significant disparities emerging between low-income individuals living in expansion states and those living in non-expansion states, particularly in the southern region of the U.S.—which could continue to widen treatment disparities.
Video Snapshots: Lessons from the Field: Centering Community Voice
PHI’s Build Healthy Places Network shares insights from experts in the community development, health and finance sectors, who are uplifting practices that support community engagement processes and projects that are community-led and owned.
In this video series, PHI’s Build Healthy Places Network features quick, deep dives with experts from the community development, health, and finance sectors. Lessons from the Field: Centering Community Voice uplifts practices that support community engagement processes and projects that are community-led and owned. Learn from practitioners from across sectors, who together are working to make neighborhoods healthier by centering the voices of residents.
Video Snapshots:
Snapshot 4: How the Affirmatively Furthering Fair Housing rule can advance racial and health equity
The Affirmatively Furthering Fair Housing (AFFH) rule was published in 2015 requiring housing authorities, local, and state governments to advance housing equity and create more opportunities for disinvested neighborhoods. In January, the Department of Housing and Urban Development (HUD) announced the new proposed AFFH rule in which participants must take meaningful steps to address housing discrimination and engage community members in decision-making processes that will help communities achieve housing equity and improve their health and well-being.
In the first interview, Build Healthy Places Network’s Co-Executive Director Colleen Flynn speaks with Will Dominie, the Housing Justice Program Director from Human Impact Partners, a national non-profit that transforms the field of public health to center equity and build collective power with social justice movements.
During their discussion, Will shares why his organization is prioritizing the proposed changes to the Affirmatively Furthering Fair Housing (AFFH) rule. He also highlights the discriminatory practices and inequitable opportunities that BIPOC communities experience and how these changes can uplift community voices and increase self-determination to address inequities and create healthier futures.
In the second interview, Rasheedah Phillips, the Director of Housing from PolicyLink, a national research and action institute dedicated to advancing economic and social equity, shares the history of the AFFH rule and why access to fair and affordable housing advances racial equity. Rasheedah and Colleen discuss how the new proposed rule will allow community members to advocate for policies in their communities that will help them achieve a fair and just opportunity for health.
Snapshot 3: Earning a Community’s Trust: A prerequisite for equitable community partnerships
The 10 Principles of Trustworthiness, created by the Association of American Medical Colleges (AAMC), integrates local perspectives with established precepts of community engagement to guide healthcare, public health, and other sectors such as community development as they work to demonstrate they are worthy of trust.
In this video snapshot, Build Healthy Places Network’s Co-Executive Director, Ruth Thomas-Squance, PhD, MPH, speaks with Philip M. Alberti, PhD, Founding Executive Director of AAMC. The two discuss the origins of the Principles for Trustworthiness, why the process is as important as the product, and how the tool applies to multi-sector efforts committed to long term relationships, where resources are shared and decisions are made collectively.
Snapshot 2: Building Resident-led Solutions for Fresh Food Access: Centering Community Voice in Cross-sector Partnerships
In this 13 minute interview, Build Healthy Places Network speaks with Diane Moss, the Managing Director of Project New Village (PNV), an organization improving fresh food access in Southeastern San Diego through resident-led, community rooted experiences that stimulate collective investments in social determinants of health. PNV was also a part of BHPN’s first Community Innovations cohort.
During this discussion, Diane Moss describes PNV’s Growers Network and Mobile Farmers Market role in creating more equitable food access in San Diego. She also provides some insights into the centering community voice while working with partners like large healthcare organizations to address food insecurity.
Snapshot 1: Lessons from the Field: Centering Community Voice
To launch the series, Build Healthy Places Network’s Co-Executive Directors Ruth Thomas-Squance and Colleen Flynn share the impetus to create this new series, including the organization’s priority to center racial equity in community investments. The two discuss how community-led approaches where residents can identify, co-create, and have an ownership stake in the solutions, can help shift community power and provide an opening to address and repair the damage of structural racism.
Videos: How to Engage Youth in Opioid Use Prevention
In these videos from the 2022 National Overdose Prevention Leadership Summit, learn how public health leaders are working alongside communities to address the youth opioid crisis.
In December 2022, over 400 leaders across 42 states convened for PHI and partners’ 4th annual National Overdose Prevention Leadership Summit (NOPLS) to discuss topics addressing the opioid crisis in the United States, including learning from youth and people with lived experiences.
In these videos from the 2022 National Overdose Prevention Leadership Summit, hear how public health leaders are working to address the youth opioid crisis.
Hearing from Youth: The Spectrum of Risk
Young people encounter a wide range of risks as they navigate the pressures and social stimuli associated with increasing independence. In addition to known risks related to ongoing substance use during the teenage years, the rise of fentanyl-laced illicit pharmaceuticals is driving a rise in youth overdose among young people during their first or early encounters with drugs. This panel was focused on sharing experiences from youth in the field and helped identify conditions and behaviors that create risk for youth. They also explored ways to promote life-saving youth engagement in programs and services.
Communities Engage Youth and Get Results by Taking Action
Empower Watsonville is a community of passionate youth who support each other and build each other up. Participants learned about how Empower Watsonville formed their coalition and how they engaged youth leaders. Crystal Gonzalez and Sofia Cuentas shared reflections on Empower Watsonville’s lessons learned about how to be effective as a coalition.
Work With Us
You change the world. We do the rest. Explore fiscal sponsorship at PHI.
Support Us
Together, we can accelerate our response to public health’s most critical issues.
Find Employment
Begin your career at the Public Health Institute.