Telehealth Policy Webinar Series: Crossing State Lines
In the fall of 2022, the PHI’s Center for Connected Health Policy (CCHP) held two webinars in its popular state telehealth policy series that focused on what the telehealth policy landscape may look like in a post-public health emergency environment. Rather than focus on individual states’ policies as examples, the two webinars explored issues that have more of a regional or national impact.
VIEW & DOWNLOAD THE WEBINAR SERIES SUMMARY REPORT
Webinar #1: Crossing State Lines – October 21, 2022
Speakers for the Crossing State Lines webinar focused on the myriad of policy considerations providers would need to consider when treating patients in another state. The expert panel included:
- Kimberly Horvath, JD, Senior Attorney, American Medical Association
- Jeremy Sherer, Esq, Partner, Digital Health Co-Chair, Hooper, Lundy, & Bookman, PC
- Kathy Wibberly, PhD, Director, Mid-Atlantic Telehealth Resource Center
Such issues like licensure are commonly known, but speakers also delved into issues around reimbursement, prescribing, malpractice insurance and consent. Due to the differences among states, providers will need to be aware that policies that are familiar within their own state are not necessarily replicated in other jurisdictions.
Webinar #2: Federal Policy & Telehealth: What to be Aware of Going Forward – October 28, 2022
For the second webinar, panelists focused on what could be expected in a post public health emergency (PHE) environment. (Please note that since the webinar took place, some changes to federal policy have occurred. Check CCHP’s website for more information). Additionally, panelists also focused on issues that policymakers have also been examining recently including concerns over waste, fraud and abuse as well as situations or conditions where telehealth can be utilized appropriately and where it cannot.
John W. Gordon, Office of Evaluation and Inspections from the Office of Inspector General (OIG) spoke about several reports recently published by the agency who has, among other items, been examining the waste, fraud and abuse issues. Carly L. Paterson, PhD, MPH, RN, Associate Director, Healthcare Delivery and Disparities Research Program, from Patient Centered Outcomes Research Institute (PCORI) discussed some of the research that organization has been involved in. Overall, all panelist noted that there is still much to be examined and that it is highly likely future changes in policy will impact the direction on some of this additional research as well as how providers continue to use telehealth.
Data Equity Webinar Series: Recordings and Resources
In Fall 2022, PHI’s Public Health Alliance of Southern California and PHI’s Center for Wellness and Nutrition hosted a four-part webinar series exploring the connections between data and equity. Watch the webinar recordings and find related resources:
- Session 1: A Race and Place Approach to Advancing Health Equity and Racial Justice
- Session 2: Best Practices in Transforming Data into Policy Actions for Health Equity and Racial Justice
- Session 3: Decolonizing Data Practices through Indigenous Evaluation Approaches
- Session 4: Data and Health Equity: Using Open-Source Data and Mapping to Understand Rural Community and Special Population Needs
Session 1: A Race and Place Approach to Advancing Health Equity and Racial Justice
The Public Health Alliance of Southern California focuses on the benefits of taking a race and place approach to examining health inequities. Using both race and place to address the impact of structural racism on health outcomes is critically important and is firmly supported by the data. The webinar also covers why examining both race and place are critical for promoting health equity.
View the Recording | Slides English (PDF) | Slides Spanish (PDF) | Q&A Fact Sheet (PDF)
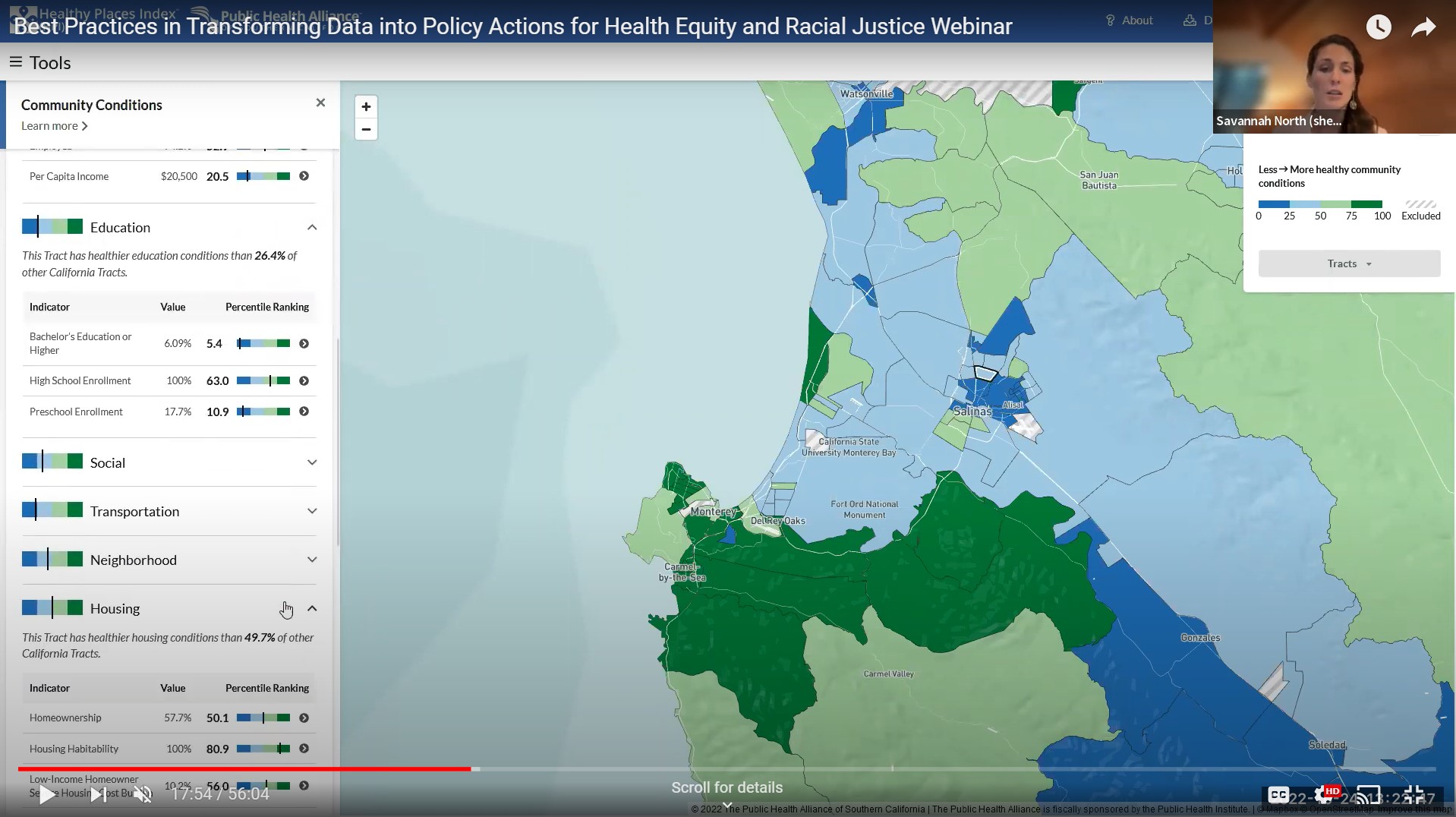
Session 2: Best Practices in Transforming Data into Policy Actions for Health Equity and Racial Justice
The Healthy Places Index (HPI) is powerful data, mapping and policy platform created by PHI’s Public Health Alliance Southern California, designed to identify opportunities to improve neighborhood health and help guide investments, programs, and policy changes to where they will have the strongest impact on life expectancy. These policies are applicable in localities and states around the country. Join PHI’s Center for Wellness and Nutrition and our Public Health Alliance Southern California to learn how to use the HPI to find policies and best practices to reduce health inequities in your community.
View the Recording | Slides English (PDF) | Slides Spanish (PDF) | Q&A Fact Sheet (PDF)
Session 3: Decolonizing Data Practices through Indigenous Evaluation Approaches
This Webinar focuses on the needs and benefits of Decolonizing Evaluation practices within public health organizations and introduces Indigenous Data Sovereignty as the right of Indigenous peoples to govern the collection, ownership, and application of data about their communities, peoples, lands, and resources. This training highlights organizational policies and practices that can be adopted to support evaluation strategies rooted in racial equity, as well as approaches to authentically engage and collaborate with Indigenous populations to support their control over how public health data and knowledge will be generated, analyzed, documented, and disseminated.
View the Recording | Slides English (PDF) | Q&A Fact Sheet (PDF)
Session 4: Data and Health Equity: Using Open-Source Data and Mapping to Understand Rural Community and Special Population Needs
This webinar describes barriers and proposed solutions for using data in addressing health inequities in rural populations. The Northwest Center for Public Health Practice has developed a dashboard to make relevant data readily available, supported by training modules focusing on using data to achieve rural health equity. This training introduces the modules and opportunities for further learning and provides examples for how data can be used to understand rural health inequities and how to address them.
View the Recording | Slides English (PDF) | Slides Spanish (PDF) | Q&A Fact Sheet (PDF)
This project was supported by funds made available from the Centers for Disease Control and Prevention, Center for State, Tribal, Local and Territorial Support, through cooperative agreement OT18-1802, Strengthening Public Health Systems and Services Through National Partnerships to Improve and Protect the Nation’s Health award #6 NU38OT000303-04-02. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by CDC/HHS, or the U.S. Government.
Video Library: How Hospitals Can Increase Access to Medication for Addiction Treatment
Explore PHI’s CA Bridge on-demand video library of training sessions to expand and deepen your knowledge of treating individuals using the CA Bridge medication for addiction treatment (MAT) method.
PHI’s CA Bridge is transforming addiction treatment by ensuring that every hospital in California provides 24/7 access to evidence-based care, treating substance use disorder like any other life-threatening condition.
Explore CA Bridge’s video library to find recorded trainings and resources to help emergency departments (EDs) and hospitals increase access to Medication for Addiction Treatment (MAT).
Browse the Video Library
The videos are designed for clinicians and substance use navigators (SUNs), and cover clinical treatment; navigation to care; and culture of harm reduction. Search dozens of videos by topic, implementation level or your professional designation. Explore and review past training sessions to expand and deepen your knowledge, including:
- “But we don’t have an opioid problem”: Breaking Down Barriers and Finding Buy-in Where There Is None
- Culture of Care: Saving Lives Through Substance Use Disorder Treatment
- The Nuts and Bolts of Rapid MAT via Telehealth
- Stigma and Inequity in OUD Care
- Trauma-Informed Care for Navigators
- Connecting Patients to On-Going Care
Podcast: PHI’s Linda Rudolph on Climate Change-Driven Health Impacts and Solutions
In this Healthy Living Healthy Planet Radio podcast interview, PHI’s Linda Rudolph discusses the health implications that come with climate change and how public health leaders are promoting equitable solutions to help mitigate and adapt to climate change.
Climate change is a global public health crisis. To help communities prepare, public health experts are working alongside local leaders to find new and creative ways to mitigate and adapt to the adverse effects of climate change.
In this episode of Healthy Living Healthy Planet Radio, host Bernice Butler speaks with Sam Calisch with Rewiring America; Debbie Ley with the Energy and Natural Resources Unit of the United Nations Economic Commission for Latin America and the Caribbean; and Dr. Linda Rudolph, program director of PHI’s Center for Climate Change and Health. Dr. Rudolph shares insights on how climate change is already creating a negative environment and health impacts—especially for our most vulnerable populations including seniors, children, pregnant women, communities of color, farmworkers and low-income communities.
Listen to the full podcast or watch the YouTube recording below to learn more about how public health leaders are working to find climate solutions that promote health and health equity.
Also available on Spotify, Google Play, Anchor, Radio Public, Apple Podcasts and Stitcher.

Doctors and public health leaders across the country are advocating for the policies that we know are going to make a difference for our health and for the climate and that's at a local level and a state level and at a federal level… trying to make sure that our climate solutions are also the solutions that promote health and health equity.Linda Rudolph, MD, MPH
Program Director, PHI’s Center for Climate Change and Health

Climate change really is a health emergency… we're seeing heat illness and deaths from extreme heat, lung and park impacts from wildfire smoke, increases in vectorborne diseases, like Lyme disease or West Nile virus, injuries and displacement from people's homes from extreme storms and flooding, more challenges with access to clean drinking water, failing crops that are making food prices rise and we're seeing more and more people, especially young people who are experiencing mental health impacts like anxiety and depression because of concerns about climate change and the future. We're seeing these effects, especially in our most vulnerable populations, seniors, children, pregnant people, communities of color and low-income communities.Linda Rudolph, MD, MPH, program director of PHI’s Center for Climate Change and Health
Webinar: Monkeypox in the Bay Area and Beyond
Monkeypox is now an international, national, and state public health emergency. Watch the August 2022 webinar featuring public health experts discussing the crisis, hosted by the Bay Area Global Health Alliance and UCSF Institute for Global Health Sciences, and moderated by PHI President and CEO Dr. Mary A. Pittman.
Monkeypox is now an international, national, and state public health emergency, made worse by an exhausted health workforce fighting stigma and misinformation, inequities in testing and care and inadequate public health funding. In order to stop the spread, we need strong partnerships—at the community level and with the private sector—especially in building trust. Innovation in surveillance and treatment are also essential.
In August 2022, the Bay Area Global Health Alliance and UCSF Institute for Global Health Sciences hosted a webinar featuring public health experts to discuss the crisis, moderated by PHI President and CEO Dr. Mary A. Pittman.
Webinar Highlights
“There are inequities in treatment, vaccines, communication, and contact tracing,” said Peter Chin-Hong, UCSF Professor of Medicine. “There are lots of challenges in equity, in terms of who is getting tested. To ask for an Mpox test, you have to say essentially ‘I’ve had multiple sex partners, I’m open with my sexuality’, and that may be limiting who is going to get a PCR test.”
“What we are experiencing here at PRC, not only at the community level with our clients, but with many of our staff, is heightened trauma and PTSD. There’s heightened suspicion among and throughout the community, great amounts of fear, often that is because of the lack of knowledge and understanding,” said Brett Andrews, Positive Resource Center (PRC) CEO.
Stigma and a lack of trust are two reasons why community wastewater surveillance is an innovative approach to detect infectious disease and inform response, said Michele Barry, Stanford Center for Innovation in Global Health Director and Alliance board member. “It gives you the ability to evaluate community health with much less bias if people are stigmatized and don’t go in for individual testing. Case identification may be difficult when you don’t see an obvious rash,” said Barry. (Stanford-based initiative WastewaterSCAN monitors wastewater for COVID-19, monkeypox, and other infectious diseases to help guide public health responses.)
Multiple, simultaneous public health crises [monkeypox and COVID-19], coupled with a lack of public health resources, have caused overwhelming challenges, including a “bone tired” public health workforce, commented Sara Cody, Santa Clara County (SCC) Health Officer and Public Health Director.
“Public health budgets have shrunk and public health workforces have shrunk over the last 10 to 15 years,” continued Cody. “While there have been many investments in healthcare delivery, there not only have not been investments in public health, but there have been disinvestments in public health.” She emphasized that flexible and consistent public health funding is essential for building the optimal health system infrastructure.
In caring for the health and safety of a large, international workforce during public health crises, Huma Abbasi, Chevron’s Chief Medical Officer and Alliance board member, noted that key to Chevron’s approach was to address misinformation and stigma through tailoring communications, activating monitoring and surveillance, repurposing materials for efficiency, continually improving established processes, and establishing strong partnerships.
“In our journeys through HIV and COVID-19, we saw that partnerships were important and have always been important,” Huma Abbasi, Chevron’s Chief Medical Officer and Alliance board member explained. “Be proactive in engaging with the key stakeholders and the business partners.”
Clarissa Ospina-Norvell, San Francisco Community Health Center’s Medical Director, agreed that partnerships have been equally valuable on a local level. “We are utilizing peer ambassadors to help educate the community and now collaborating with other service providers, and our immediate community in the Tenderloin, to bring the vaccines to them,” said Ospina-Norvell when speaking about how the San Francisco Community Health Center is addressing monkeypox.
May 2022 marked the first time that many monkeypox cases and clusters have been reported concurrently in non-endemic and endemic countries in widely disparate geographical areas. It is a global health challenge facing the Bay Area and beyond.
Speakers:
-
George Rutherford – UCSF Professor, Epidemiology & Biostatistics; Director, Prevention and Public Health Group; Acting Director, IGHS
-
Dr. Peter Chin-Hong – UCSF Professor of Medicine
-
Sara Cody – Santa Clara County Health Officer and Public Health Director
-
Michele Barry – BAGHA board member; Stanford Professor of Medicine; Director, CIGH of the Center for Innovation in Global Health and Senior Associate Dean for Global Health
-
Brett Andrews – SF’s Positive Resource Center (PRC) CEO
-
Clarissa Ospina-Norvell – SF Community Health Center’s medical director
-
Huma Abbasi – Chevron’s Chief Medical Officer and BAGHA board member
-
Mike Steinberg – Chevron’s Team Lead of Global Public Health and Special Projects
Moderator:
-
Mary Pittman – Public Health Institute’s CEO and BAGHA board chair
Telehealth & Medicaid: A Summer 2022 Policy Webinar Series & Summary
In the summer of 2022, PHI’s Center for Connected Health Policy (CCHP) held its fourth Medicaid and State Telehealth Policy Webinar series. While previous series have usually focused on Medicaid policy, the Summer Series took a different track by examining other telehealth policy issues that are in the jurisdiction or have a significant impact on state policy.
2022 Summer Series Webinar Topics
- Telehealth in School-Based Programs
- Telehealth and Licensure
- Private Payer Telehealth Laws
- Telehealth and Substance Use Disorders
Panelists included a wide-range of experts and policymakers including representatives from state Medicaid programs, federal, state, and local agencies, health plans, legislative representatives and patient advocates. Each speaker brought their unique perspective, knowledge and experience providing attendees a well-rounded discussion and background on each topics.
Watch the webinar recordings and see highlights (below), or download CCHP’s summary report of the entire series.
Medicaid & State Telehealth Policy: School-Based Telehealth
This webinar is a part of CCHP’s Medicaid and State Telehealth Policy webinar series and will focus on the use of telehealth to deliver services in a school-based program. Learn how Medicaid and Education departments work together to ensure children receive the services they need. See additional resources from the webinar.
Medicaid & State Telehealth Policy: State Licensure
Licensure has often been cited as a barrier to the use of telehealth. With the possibility of COVID waivers expiring, the exemptions given to licensing requirements are beginning to disappear. This webinar will focus in on what the post-PHE landscape will look like and what are some of the methods that are being utilized to address the licensure issue. See additional resources from the webinar.
Medicaid & State Telehealth Policy: Telehealth Private Payer Laws
The majority of states have passed laws impacting private health plans’ coverage of telehealth-delivered services. This webinar will focus on the path of these laws by looking at how one came into being with legislation, how a health plan implements and reaction to such a policy and does the entity that would enforce such a law have to say. See additional resources from the webinar.
Medicaid & State Telehealth Policy – Medicaid Telehealth Policy & Substance Use Disorder
In addition to COVID-19, the United States faced another public health crisis, the opioid epidemic. During COVID-19, some substance use disorder (SUD) patients found themselves cut off from care. Telehealth was used to help alleviate some of these access issues. In this webinar, we’ll hear about various approaches to the use of telehealth to treat SUD from federal, state and local perspectives. See additional resources from the webinar.
Videos: What Latino Parents Need To Know About COVID Vaccines
What do Latino parents need to know about COVID and vaccines to help protect the health of their kids, families and communities? How can doctors and other medical providers communicate more effectively with the Latino community about the pandemic, vaccines and other health and safety measures?
In this video series, PHI’s Latino Coalition Against COVID-19 answers frequently asked questions about COVID vaccines in English and Spanish. It also includes recommendations and best practices for the medical community to reach Latino parents and families.
The videos feature:
- Dr. Ilan Shapiro, Chief Health Correspondent Medical Officer, Alta Med
- Dr. Eloisa Gonzalez, Director, Cardiovascular and School Health Los Angeles County Department of Public Health
- Dr. Daniel Turner-Lloveras, Executive Director, The Latino Coalition Against COVID-19
- Enriqueta Guido, LCAC19 Community Member
- María Guido, LCAC19 Community Member
Find FAQ videos in Español and English below, or watch the Youtube playlist to see the full series.
What Latino Parents Need To Know about COVID Vaccines / Lo Que Los Padres Latinos Necesitan Saber
A Virtual Q&A / Una Q&A Sobremesa Virtual
Español
Estoy confundido sobre el plan para vacunar niños menores de 5 años. ¿Puedes explicar?
¿Que significa si el ensayo clínico en niños no dio resultados similares a los adultos?
Me vacuné, tuve covid, y estoy recuperado ¿puedo regresar a la normalidad?
¿Por qué debo vacunar a mi hijo si el COVID solo causa una enfermedad leve?
¿Qué pasa si mi hijo(a) cumple 12 años entre la 1a y la 2a vacuna?
¿Y que le dijo a las personas que decian que era malo?
¿Que fueron algunas de las cosas que escucho sobre la vacuna que no pensaba que era verdad?
¿A la larga, recibirán los niños dosis de refuerzo como los adultos?
¿Por qué se recomienda la inyección de refuerzo contra el COVID-19?
¿Qué es una inyección de refuerzo?
No hay muchos niños que se están enfermando, ¿es necesario vacunarlos? Dr. Ilan Shapiro
¿Cómo pueden los padres decidir si deberían vacunar a sus ninos? Dr. Ilan Shapiro
¿Para que voy a recibir la vacuna si todavia me podria enfermar?
¿Conoces a alguien que haya muerto de COVID-19?
Enriqueta Nos Habla Sobre Su Experiencia Con Las Vacunas de COVID-19
¿Tuvo alguna duda antes de recibir la vacuna para prevenir el coronavirus-19?
¿Usted o alguien de su familia se enfermó de coronavirus-19?
English
What Latino Parents Need To Know COVID Vaccines / Lo Que Los Padres Latinos Necesitan Saber Premiere
A Doctor’s Personal Story: How to talk to family about COVID-19 vaccines
Do you anticipate boosters will be recommended for the 5-to-11 age group?
Why should I vaccinate my child if they already had COVID-19?
I’m vaccinated, boosted, and had covid-19, can I go back to normal?
There have been conflicting reports about vaccinating kids, how does this all work? Dr. Ilan Shapiro
Why should I vaccinate my child if COVID only causes mild illness?
How To Approach Latino Parents About COVID-19 Vaccines. Dr. Gonzalez & Dr. Turner-Lloveras
My family member is ill with COVID-19, are there treatments I can use at home?
What does it mean to be “fully vaccinated” now?
I’ve been suffering prolonged COVID-19 symptoms. Do I have Long COVID? How should I ask my doctor?
Should I ask my doctor for monoclonal antibody treatment if I have COVID to prevent hospitalization?
Lo Que Importa Ep. 3 | How To Get Back To Normal Without Being Done (English)
What does it mean, the clinical trials in children were not as strong as in adults? Dr. Ilan Shapiro
How should parents decide if they should get their child vaccinated? Dr. Ilan Shapiro
There aren’t that many kids getting sick, is it necessary to vaccinate your children?
Video: PHI STAR Fellow Dr. Olayinka on Gates Foundation Working Dinner: “New Variants, New Challenges”
From flattening the curve to riding the waves, variants have shaped the entire pandemic and will shape our future. How does the world better prepare?
In the third episode of the Gates Foundation Working Dinner series, global health leaders Dr. Folake Olayinka, a fellow with PHI’s STAR program, and Dr. Samba Sow join Anita Zaidi and Keith Klugman to discuss how COVID-19 variants altered the trajectory of the pandemic and share their thoughts on how to better prepare for both future variants and the next pandemic—beginning at the community level.
Dr. Olayinka emphasizes that globally, no one is safe until we all are safe. We need vaccine and health systems and infrastructure to make sure vaccines are not only available and can be delivered into people’s arms; we need to ensure those systems and infrastructure are in place long term to help us fight the next pandemic.

It’s not good enough for those [health] systems to be in some places. They’ve got to be in all the places, because what this pandemic has really shown us is that we’re all at risk.Dr. Folake Oliyanka
Global health specialist and STAR Fellow, Public Health Institute
More about PHI’s Sustaining Technical and Analytic Resources (STAR)
STAR is a five-year USAID-funded Fellowship project that improves the knowledge and skills of US and low-and-middle-income country (LMIC) professionals and institutions engaged in global health. STAR is in partnership with the University of California, San Francisco. Learn more.
Video Series: Communicating About Vaccines
In this video series, PHI’s Berkeley Media Studies Group offers strategic communication tips to help public health advocates and practitioners communicate with the public in ways that foster trust.
Find strategic guidance, tips and examples for how public health practitioners and advocates can communicate effectively about vaccines in ways that foster trust, in this video series from PHI’s Berkeley Media Studies Group.
Communicating about vaccines: Meeting people where they are
Shame is all too common in communication about vaccines, but we should avoid it because it is not effective at changing individuals’ hearts and minds. Instead, as research has shown, we need to demonstrate empathy, listen without judgment, and share messages using credible local spokespeople who are easy for audiences to relate to. Learn more in this video, the fourth in a series from Berkeley Media Studies Group.
Transcript
Best practices in strategic communication tell us that shame is not an effective tool for changing individual behavior. This is true for any health issue, including vaccination.
PAMELA MEJIA, BMSG HEAD OF RESEARCH: When people feel shamed or stigmatized about their choices, they tend to retreat; they tend to become defensive; they stop asking questions; they close themselves off to new information. So, you can clearly see how, in the context of immunizations, shame would be very problematic.
Parents who feel that they are being shamed or branded as anti-vaxxers just for asking questions about medical treatments for their child might become very defensive, might retreat further into distrust and dislike of the medical community and vaccinations.
I think establishing trust and rapport is critical to communicating effectively about vaccines and why they matter.
NARRATOR: That begins with our messages — and our willingness to listen.
MEJIA: So, language is a really important consideration. I always advise people to try and avoid the phrase anti-vaxx or anti-vaxxer because it is stigmatizing; it is limiting; it does make people defensive and can close them off to hearing more information. There is value in using phrases like “people who are questioning” or “people who are unsure about vaccination.”
NARRATOR: It’s also important to listen without judgment when questions arise.
MEJIA: We talk about meeting people where they are — well, we really have to be in there with people to do that. It is completely normal and valid and right and to have questions, especially about something that is going into your body or the body of somebody that you love.
I would caution people who are trying to communicate about vaccines — I would caution them against pretending that misinformation doesn’t exist. To put another way, I think we just need to acknowledge that there’s a lot of information out there; we need to make people feel comfortable and heard in having questions about it, and we need to share that we’re kind of all living in this information-overload world.
NARRATOR: In an op-ed for The Cincinnati Enquirer, two co-founders of a community engagement start-up emphasize the importance of listening directly to community residents’ concerns. They held six focus groups in Ohio “to identify strategies to encourage more people to feel comfortable receiving the vaccine.” Their top lessons included acknowledging hesitancy with respect, focusing on how vaccination keeps vulnerable people safe, and using relatable local messengers.
MEJIA: There are some people who, perhaps, will never be moved on vaccinations. But there are many people who are just questioning, who just want to know a little bit more, who just need a little bit of reassurance. I think it’s important that we focus on people who, maybe are questioning but can be moved, who can — with additional information, with additional space to ask questions, with authentic messengers they can relate to — might well be moved to embrace vaccines and embrace being immunized.
Communicating about vaccines: How to discuss racial equity in vaccine uptake
To help ensure equitable vaccination rates in all neighborhoods, public health advocates and practitioners must center communities of color in their messages. Being silent on racism allows vaccine opponents to invoke medical oppression in their communication, stoking further division, hesitancy, and distrust. This video, the third in a series from BMSG, offers strategic communication tips for advancing racial and health equity in immunizations.
Transcript
[KIM GARCIA, BMSG RESEARCHER]: Communities of color have many reasons for having hesitancy around vaccines. Medical racism and medical oppression have been experienced and continue to be experienced by people of color. There’s also a lack of representation of providers — medical providers and even public health practitioners, who we see in our communities who may not look like us, and so there’s a barrier of trust that needs to be built when we don’t see ourselves or see our lived experiences represented.
[NARRATOR]: So, how do we go about building trust with community partners? For starters, public health advocates and practitioners cannot stay silent on racial inequity and the structures that create it.
[GARCIA]: To leave race out of the conversation is really leaving it up to vaccine opponents to take up that issue themselves. We found that vaccine opponents bring up instances of medical racism and medical oppression ultimately to undermine trust in the medical system. By using race to divide us, they’re turning us against each other, they’re turning us against medical providers and government overall.
[NARRATOR]: When advocates address racial equity in messages about vaccines, they must go beyond acknowledging past harms.
[SHADDAI MARTINEZ-CUESTAS, BMSG HEAD OF TRAINING]: Focusing on hesitancy has been a way to deflect responsibility for equitable distribution on the front end.
[NARRATOR]: To make sure their messages don’t reinforce hesitancy, advocates must also discuss structural barriers, many of which predate the pandemic.
[GARCIA]: Lack of health insurance, lack of transportation, lack of housing that gives someone a safe and stable place to even think about getting vaccinated in the first place. We know that, for example, even your zip code could be shaping your risk for exposure. We also we can talk about lack of protections that are in place for frontline and essential workers, who are predominantly people of color.
And so, that really points to someone in power who can put those protections in place. So, when we talk about the landscape, when we talk about the structures that can hinder people’s access to vaccines, we can then point to solutions that are structural and systemic solutions. Rather than “this person needs to be able to get a vaccine,” but, “how can we improve our structures and systems so that all people can get vaccines?”
[MARTINEZ-CUESTAS]: I want to point out an article by Politico that it is focusing on the systems instead of just blaming individuals. The chief medical executive of Minnesota has a really great quote in this article, talking about how the best public health happens when you go into neighborhoods and when you’re working with communities and how it is the duty and responsibility for public health to go to where their communities are at.
[NARRATOR]: Advocates can also advance equity by including values in their messages.
[GARCIA]: When we talk about vaccines, we’re really thinking about the greater good, our collective, our community. These are the values that we hold because we know that communities of color are being disproportionately impacted by COVID-19. Vaccine opponents, on the other hand, tend to use a very individual frame; they really look at my personal choices, my personal freedoms. That creates greater division and, if we stay silent on racial equity from a public health side, vaccine opponents will only continue to stoke those divisions.
Communicating about vaccines: Illuminating the context for access and hesitancy
To boost vaccine rates, public health practitioners and advocates need more than just compelling messages; we also must confront the practical barriers that make it hard for some people to access the vaccine — and credible information about it. In this video, the second in a series from BMSG, we discuss the context for why vaccination rates are lagging in some communities. Learn more about COVID-related communication and view other videos at www.bmsg.org/covid-19.
Transcript
[NARRATOR]: There’s no shortage of news about COVID-19 vaccination rates. Stories about state and national rankings, pockets of vaccine hesitancy, and the health consequences of being unvaccinated routinely make headlines. Less common are stories that make visible the context for whether people can easily access the vaccine and credible information about it. BMSG’s research team has gained insight into what’s missing from conversations surrounding vaccination, after studying news coverage of the issue.
[PAMELA MEJIA, BMSG HEAD OF RESEARCH]: One of my favorite quotes that came from the research that we did was from a physician who talked about vaccine deserts. So, these are places where access to vaccination sites is very, very limited: There might be very few of them; they might have limited hours, limited staff; they might be difficult to access via public transportation; they might be difficult to access financially.
Communities that have been marginalized and tend to be ignored for things like healthy food, for health care facilities, etc., they also tend to be ignored and left out of access to vaccination sites. As advocates and practitioners — as people who want to increase rates of vaccination — we have to illustrate for folks that sometimes many people want to be vaccinated, but they simply can’t.
[NARRATOR]: Although stories illustrating access issues are relatively rare, our researchers did find some good examples. In this article from The Washington Post, the executive director of the American Public Health Association explains why it’s important to expand coverage in ways that highlight practical barriers. He says, quote, “If you’ve got to take two buses and walk a few blocks, plus hesitancy, where is the incentive to go get that shot?”
Another factor hindering vaccination rates is a lack of access to trustworthy information about it.
[PAMELA MEJIA, BMSG HEAD OF RESEARCH]: There is a long history of misinformation and disinformation from vaccine-hesitant or vaccine-skeptical folks. It’s interesting that they — that vaccine opponents tend to sow a lot of distrust of medical science and medical professionals because, at the same time, they try to evoke or mimic medical professionals and medical work.
When we were doing our analysis of documents, we found a number of fact sheets from organizations like the CDC, and we also found fact sheets that looked almost identical in terms of their layout, their formatting, some of their language choices, etc., but they came from vaccine-hesitant or vaccine-skeptical organizations.
There’s no way of knowing what the individual media environment or messaging environment somebody’s been exposed to is, which makes it doubly important that we be reflective of and acknowledge access issues, and, you know, really be prepared to talk about some of the uncomfortable questions that people may have. We need each other’s help in figuring out where to go and where to ask questions and what information to trust when it comes to vaccinations.
Look at who’s providing the information — whether it’s from a reputable source or not. If data is being cited, is it coming from a reputable place, or, um, is it sourced at all? If data is presented without a citation, that’s a sign that this might not be a very good source. And look at the timeliness; look at how current the information that’s being presented is.
Establishing that there are questions, there is competing information, that there can be a lot of confusing and conflicting information in the world is an important step towards making people feel heard. It’s kind of a way of acknowledging our shared humanity.
Communicating about vaccines: Investing in trusted messengers
Transcript
[NARRATOR]: Vaccines save lives. We know that from research, but many people remain hesitant to get their shots.
To boost confidence in the vaccine, we not only need to give people access to it in places they trust, but we also need to deliver accurate information about it through trusted messengers.
[SARAH PEREZ-SANZ, BMSG RESEARCHER] Dr. Anthony Fauci is definitely an expert, but some people may think that, oh, he doesn’t know enough about my family. He’s not an expert in my kids.
[SURGEON GENERAL DR. VIVEK MURTHY]: What we have to do is not only get information out there through traditional sources and through the media; it’s working with local nurses and doctors, with teachers, with faith leaders, and others in local communities to make sure they have information that they can use to share.
[NARRATOR]: Research from the Berkeley Media Studies Group aligns with the surgeon general’s recommendation.
[PEREZ-SANZ]: So, you know, data is important. We collect data as part of our research, but stories are really what drives the data home for people. So, if someone has their own experience from going from vaccine hesitancy to having their kids or themselves fully vaccinated, that journey is really important to share with others. And while we can capture that in our research as data, it really only matters to people if you tell the story of how they went from vaccine hesitant to fully vaccinated.
Public health advocates and champions can reach out to find people who have decided to be vaccinated, and who are excited to be vaccinated, and talk to them about what being vaccinated means to them.
You can have them author op-eds, letters to the editor, you could even use them as contacts; if a reporter were to call you, you could say, “Hey, you should also talk to so-and-so because they are super excited to get vaccinated, and they have a really great story.”
[NARRATOR]: BMSG monitors the news to find out what that looks like in practice.
[PEREZ-SANZ]: This article [from The Wall Street Journal] came out right when 12- to 15-year-olds were starting to be able to be vaccinated. So, people were signing up; people were excited to get their kids vaccinated because it’s been a long year and a half. And so this article includes quotes from youth and then also parents. So, there’s just a lot of great voices in this article.
First, I want to highlight Elliott Ferris. He’s a 13-year-old, and his mom signed him up for a vaccine appointment at his pediatrician’s office. And Elliott, he was so excited, he said, quote, “That’s so dope!” and that quote “I’ve had such a long year-and-a-half without friends. We’re just so bored and a little bit lonely.”
So Elliott really speaks to the fact that, you know, he gave up a lot. He had to sacrifice a lot over this past year. Now that he will be vaccinated, he can get back to doing the things that he loves to do with his friends.
For more tips on communicating effectively about COVID-19 and vaccines, visit bmsg.org/covid-19.
Virtual Forum: “Public Health and the Delivery System: Vital Connections” featuring Mary Pittman
Watch the recordings from Kaiser Permanente’s Institute for Health Policy’s two-part virtual forum, featuring PHI President and CEO Dr. Mary A. Pittman. Hear speakers examine how public health department and delivery system leaders are navigating the pandemic response, and how we can support an effective public health system for the future.
How are public health department and delivery system leaders successfully navigating the pandemic response? How can we support an effective public health system, now and for the future?
Held in winter 2021, this two part virtual forum from Kaiser Permanente’s Institute for Health Policy explored opportunities to strengthen partnerships and collaboration between public health and the broader health care delivery system; identified barriers public health and delivery system leaders face—including financial, workforce, and infrastructure challenges—and discussed ways to ensure a well-financed and supported public health system in the future. Presenters also shared promising policy solutions to promote and improve our public health system in ways that address public health needs and advance health equity.
The discussion featured Dr. Mary Pittman, President and CEO of the Public Health Institute; Greg A. Adams, CEO of Kaiser Foundation Health Plan; Anthony A. Barrueta, Senior Vice President of Government Relations for Kaiser Foundation Health Plan and PHI Board member, and more.

Community based organizations are more than partners. They are an integral part of the public health ecosystem and we need to think about how to shift resources, power and decision making, and different ways of thinking about community based organizations and our next steps in building that important link between healthcare and public health.Dr. Mary Pittman, Part Two: Public Health and the Delivery System: Building a Stronger System for the Future
Part 2: Building a stronger system for the future
Building off the perspectives elevated in part 1, this discussion focused on how to build a stronger system in the future that improves the public’s health in an equitable way, both in public health emergencies and in the longer term.
- Mary A. Pittman, DrPH, Chief Executive Officer and President of the Public Health Institute
- John Auerbach, MBA, Director of Intergovernmental and Strategic Affairs at the Centers for Disease Control and Prevention
- David Grossman, MD, MPH, interim Senior Vice President of social and community health for Kaiser Foundation Health Plan, Inc. and Hospitals
- Cecilia Oregón, MPP, MPH, Executive Director for Kaiser Permanente’s Institute for Health Policy
- Anand Parekh, MD, MPH, Bipartisan Policy Center’s (BPC) chief medical advisor providing clinical and public health expertise across the organization.
- Lauren Smith, MD, MPH, Chief Health Equity and Strategy Officer for the CDC Foundation
Part 1: Navigating the pandemic response
In this discussion, speakers elevate perspectives from public health department and delivery system leaders to gain a clearer understanding of their experiences and lessons learned responding to the pandemic.
Part one speakers:
- Greg A. Adams, Chair and CEO of Kaiser Foundation Health Plan, Inc. and Hospitals
- Oxiris Barbot, MD, Physician, Public Health Practitioner and Innovative Leader
- Anthony A. Barrueta, JD, Senior Vice President of Government Relations for Kaiser Foundation Health Plan, Inc. and Hospitals
- Patty Hayes, RN, MN, former Director of Public Health Seattle & King County
- Stephen Parodi, MD, Executive Vice President of External Affairs, Communications, and Brand at The Permanente Federation
- Megan Ranney, MD, MPH, Warren Alpert Endowed Professor of Emergency Medicine at Alpert Medical School of Brown University and Founding Director of the Brown-Lifespan Center for Digital Health
Work With Us
You change the world. We do the rest. Explore fiscal sponsorship at PHI.
Support Us
Together, we can accelerate our response to public health’s most critical issues.
Find Employment
Begin your career at the Public Health Institute.