In the News
Black Churches in California Help Provide End-of-Life Care
- Reasons to be Cheerful
-
Focus Areas
Health Care & Population Health -
Expertise
Health Education & Promotion, Outreach & Dissemination -
Programs
AC CARE Alliance(PHI program 2018-2025)

“Planning for dying and death is a conversation most Americans avoid. Even though talking through and documenting your wishes about end-of-life medical care has been shown to benefit patients and caregivers, only about one in three US adults have created advance directives, like living wills and other legal documents that inform care when a person can’t communicate their own wishes.
As in so many aspects of the US healthcare system, there are racial disparities, too. Among older Americans, just 24 percent of Black people had advance directives according to a 2014 study, while 44 percent of white people did. That means families of color may miss out disproportionately on the benefits advance directives can provide, from giving patients a stronger voice in their own care to relieving stress on family members.
A program in Oakland, California set out to change this — and has recently expanded to Los Angeles on the strength of its positive results.
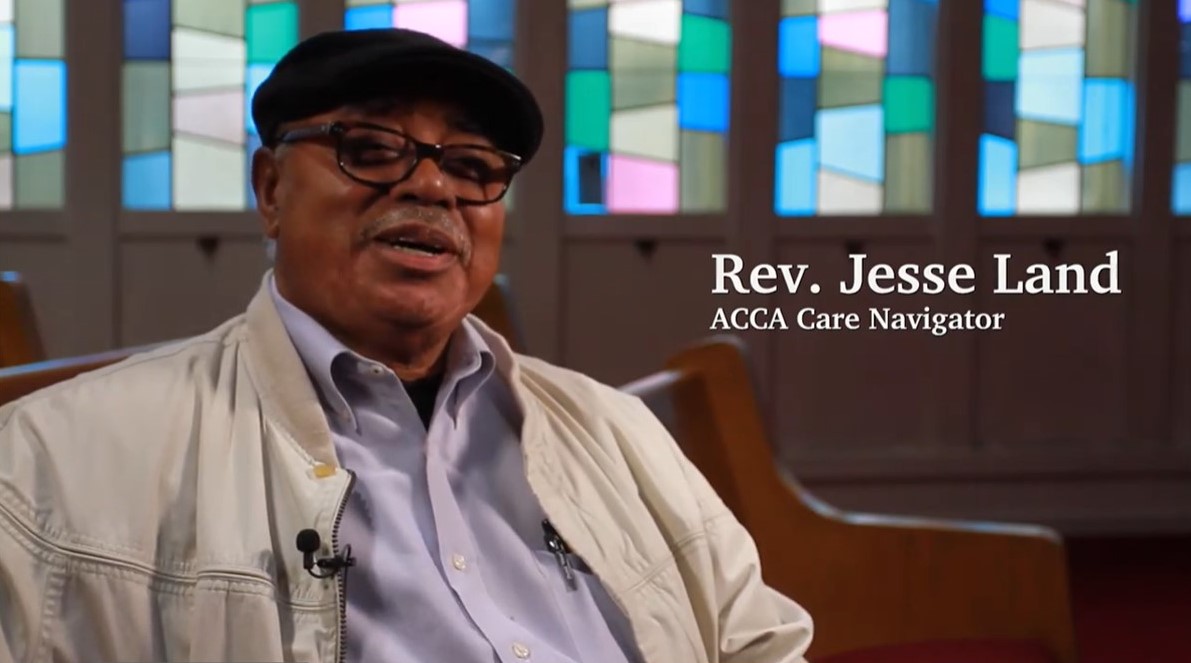
Since 2015, the Alameda County Care Alliance has run a free Advanced Illness Care Program (AICP). Founded with local Black churches, the program offers individualized support for people with advanced illnesses and their caregivers. AICP’s trained care navigators belong to the same communities as the participants, helping to build trust in people often wary of the intentions of medical care and research systems.
With five to 12 meetings over six months, care navigators provide structured guidance and assistance in navigating a variety of life issues, from helping locate social services to working through the disquieting questions necessary to create advance directives.
AICP has served more than 1,600 patients and caregivers so far. Three-quarters of participants have been African American, and 55 percent — far above national averages — have gone on to complete advance directives.
Navigating quality of life
Most clients hear about AICP through local churches, whose leaders were instrumental in identifying the need for a program that creates a bridge between church and health care for those facing advanced illness.
The average age is late 60s, but clients have ranged in age from 35 to 101, as illness can strike at any time and caregivers may be younger family members. In some cases, when impairments like dementia or stroke render patients less able to interact, the primary client is the caregiver.
AICP care navigators are trained to offer guidance in several areas: health, spiritual, social, caregiving and advance care planning.
For instance, they help clients get what they need out of doctor visits.
“The clinical visit tool helps them organize their thoughts: ‘What do I want to ask the doctor, what do I want to tell the doctor, and what do I want the doctor to do?’” says care navigator Jae Williams, who joined the AICP team in 2021.
To help, the AICP team created a detailed, 23-page Care Planning Workbook, designed with the input of ACCA leadership, care navigators and pastors. The workbook, which also is available to the public as a free download, includes information on what end-of-life treatments are available and guidance on how to have discussions with family, friends and clinicians and select a health care agent.
The workbook’s initial questions prompt people to identify simple things that make life worth living. For some, Williams says, that might be knowing their great-grandchildren or being able to get outside every day. And that discussion opens a path to some deeper and more difficult questions.”
To read the full article, click on the link below.
Originally published by Reasons to be Cheerful
More Updates
Work With Us
You change the world. We do the rest. Explore fiscal sponsorship at PHI.
Support Us
Together, we can accelerate our response to public health’s most critical issues.
Find Employment
Begin your career at the Public Health Institute.