In the News
NY Times Magazine Features PHI’s Bridge Center on Buprenorphine as an Effective Treatment for Opioid Addiction
- The New York Times Magazine
-
Focus Areas
Health Care & Population Health -
Expertise
Coalition & Network Building, Health Education & Promotion, Quality Improvement -
Programs
Bridge, CA Bridge

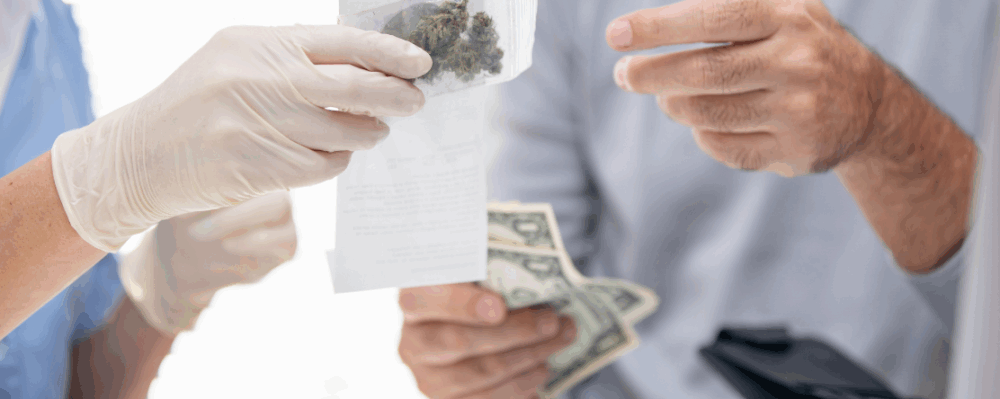
In this New York Times Magazine piece, writer Moises Velasquez-Manoff spent 18 months observing PHI’s Bridge model at Highland Hospital in Oakland, CA, where he interviewed experts from PHI’s Bridge Center and their networks for this in-depth story on how to curb the opioid epidemic. PHI experts Dr. Andrew Herring and Dr. Aimee Moulin highlight the Bridge model which works to transform addiction treatment by ensuring that every hospital provides 24/7 access to evidence-based medication for addiction treatment, substance use navigators, and connections to ongoing care in the community. In the article, both Herring and Moulin discuss why more clinicians aren’t prescribing buprenorphine when research shows that medication for addiction treatment is highly effective and can significantly reduce the risk of overdose death.
The middle-aged patient seemed to embody all the twists and contradictions of the opioid crisis. A white-collar professional with a history of addiction, he had become hooked on prescription painkillers again after a knee operation. When doctors would no longer prescribe the opioids, he returned to heroin. But recently he had developed an abscess at an injection site on his leg. Now he was in Highland Hospital, in Oakland, Calif., claiming to have been bitten by a spider.
Andrew Herring, a specialist in emergency medicine at the hospital, vividly remembers this man, the first person he would ever treat with the drug buprenorphine. The patient was hoping to receive a few opioid pills to help with his “spider bite.” But he had also caught wind of a trial program Herring was just then starting in the emergency department. He and his colleagues were interested in buprenorphine — itself an opioid — as a way to treat addiction to more powerful opioids like heroin. The patient wanted to try that instead of attempting to finagle pills. Struck by his forthrightness and honesty, and by his evident desire to escape the downward spiral of addiction, Herring sent him home with a prescription.
This was in 2016. The previous year, doctors at the Yale School of Medicine published what would come to be seen as a seminal study in the field of addiction medicine. Their study subjects, primarily people who were using heroin or prescription opioids, had been divided into three groups. One received a referral to addiction-treatment services outside the hospital. Another group received a similar referral, along with a brief counseling session at the hospital. And a third group received both the referral and the counseling while also starting on buprenorphine, taken daily as a tablet. After a month, this last cohort was about twice as likely as the other two groups to remain in treatment. This one medicine doubled these patients’ likelihood of staying the course and greatly improved their odds of avoiding a fatal overdose.
An unusual aspect of the study was its setting: the emergency room. Addiction treatment usually didn’t happen in the emergency department, a place generally seen as reserved for acute medical issues, not disorders like drug addiction that require long-term treatment. Yet Herring couldn’t stop thinking about the implications of the Yale research — about how many lives might be saved if E.R. doctors embraced this approach.
And there was already evidence of buprenorphine’s effectiveness, at the population level, in combating overdose deaths. Although the United States government had partly funded buprenorphine’s development as a treatment for opioid addiction, France was one of the first countries to most fully exploit the drug’s potential. In the 1990s, French health authorities began allowing any doctor to prescribe buprenorphine. By the early 2000s, overdose deaths there from heroin and other opioids had declined by nearly 80 percent.
Intrigued by this and other evidence, Herring, who was head of emergency-medicine research at Highland, decided to try the drug in his own E.R. Its transformational potential was quickly apparent. Opioid users often arrived in the E.R. in withdrawal — sick to their stomachs, cranky, itchy, mean. Doctors and nurses dreaded dealing with them. But when Herring gave these patients buprenorphine, their pain and nausea subsided quickly. Herring could sense human warmth where before he was seeing only anguish. “This is why I became a doctor,” he says he recalls thinking. “It really does feel like a restoration of health.” (The middle-aged patient who claimed to have a spider bite got his life in order and eventually moved abroad.)

This is why I became a doctor. It really does feel like a restoration of health.Andrew Herring, MD
Program Director, Bridge Center, Public Health Institute
That same year, Herring and his colleagues established what is now called the Alameda Health System Bridge Clinic, an addiction-treatment program that has since become a model for hospitals and physicians in California and other states. In the decade that followed, the scourge of opioids only worsened. In 2022, more than 107,000 Americans died from drug overdoses, most of them from fentanyl, a fatal-overdose rate nearly quadruple what it was 20 years earlier. More people died from opioid overdoses in that period — more than 700,000, according to C.D.C. data — than perished in all U.S. wars and conflicts going back to World War I.
Over time, opioid users have transitioned from taking prescription drugs like OxyContin to heroin to the fentanyl that now dominates the illicit drug market. The epidemic has crested in different communities at different times. Initially, white Americans died in the greatest numbers. But around 2020, death rates among Black Americans caught up with and then surpassed those of their white counterparts. Today the opioid crisis disproportionally kills African Americans and Native Americans.
Many see illicit fentanyl, said to be about 50 times as powerful as heroin and 100 times as powerful as morphine, as the worst drug epidemic the country has ever seen. At the same time, experts have reached a consensus: Medication-for-addiction treatment, or M.A.T. — using medicine like buprenorphine or methadone to help patients recover from their opioid-use disorder rather than trying to get them to quit cold turkey — is the best course of treatment. Merely starting people on buprenorphine, research suggests, can cut their chances of dying from overdose by between 50 and 80 percent, compared with patients receiving talk therapy and other nondrug interventions. Yet the drug remains drastically underprescribed.
Herring and others around the country are on a mission to change all this. One goal at A.H.S. Bridge is to demonstrate that, contrary to still-pervasive assumptions, a good treatment for opioid addiction exists — and that doctors can deploy it easily in their emergency departments. “Our big project,” Herring says, “is to free buprenorphine.”
Outside the entrance to the emergency department where Herring works in Oakland sits a metal dispenser not unlike those that, where they still exist, give out alt-weekly newspapers. This dispenser contains free boxes of naloxone, the overdose-reversal drug also known as Narcan, for anyone who wants it. “That’s how we start,” Andrew Herring told me one fall day. Making the drug more widely available around the country may be paying dividends already. In 2023, according to C.D.C. data, fatal overdoses declined nationally for the first time since 2018.
But for Herring, it is buprenorphine, a drug fewer people have heard of, that can be the true lifesaver. Unlike naloxone, which only helps in the moment of acute, opioid-induced emergency, buprenorphine can get someone started on a durable recovery — and the drug is safer than most other prescription opioids. Its lack of toxicity stems partly from its unique action in the body. As an opioid itself, buprenorphine excites opioid receptors, preventing withdrawal symptoms. But unlike with other opioids, including methadone, which is also used to treat opioid addiction, there’s a limit to how much buprenorphine can stimulate those receptors. That ceiling protects against overdose. The molecule is also unusually “sticky” on those receptors — more so than both heroin and fentanyl, for example — so flooding the body with buprenorphine can block the effects of more potent opioids that patients going through a relapse might procure on the street. In the last decade, the F.D.A. approved new forms of the drug that can be given as a shot weekly or even once a month, so patients can avoid the hassle of having to take it daily.
At A.H.S. Bridge, patients can be treated with buprenorphine minutes after they show up, right inside the emergency room, not in some distant wing of the hospital. And the program forgoes nearly all the initial paperwork for people with substance-use disorder. “You can’t take care of unhoused people if you’re futzing around with insurance cards,” Herring said.
The Bridge clinic’s nerve center is a room full of administrators called “substance-use navigators.” These navigators locate long-term treatment programs, follow up on prescriptions, connect patients with the correct doctors for their other health problems, remind patients about appointments and generally try to keep them engaged in their own care.
Click on the link below to read the full article.
Originally published by The New York Times Magazine
More Updates
Work With Us
You change the world. We do the rest. Explore fiscal sponsorship at PHI.
Support Us
Together, we can accelerate our response to public health’s most critical issues.
Find Employment
Begin your career at the Public Health Institute.



