
California Pregnancy Mortality Surveillance System Factsheet: Pregnancy-Related Mortality, 2018–2020
- Christy McCain, MPH
- Paula Krakowiak, Dan (Susan) Sun, Deepika Mathur, Christine H. Morton, Kimberly Gregory
-
Focus Areas
Health Care & Population Health, Women, Youth & Children -
Issues
Reproductive & Sexual Health -
Expertise
Research – Quantitative, Research – Surveillance -
Programs
California Pregnancy-Associated Mortality Review

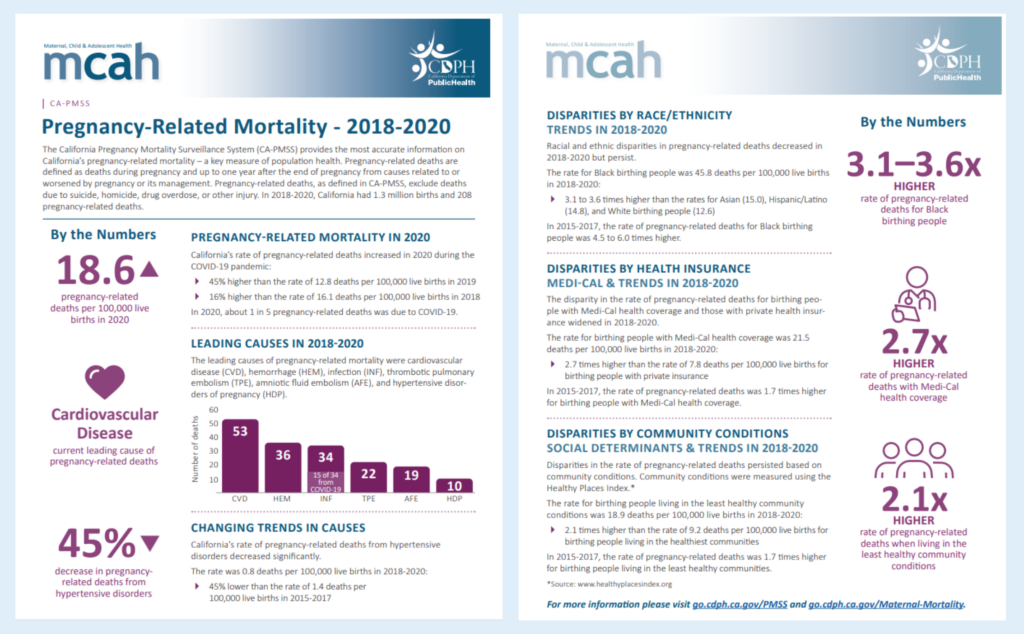
The California Pregnancy Mortality Surveillance System (CA-PMSS) provides the most accurate information on California’s pregnancy-related mortality—a key measure of population health.
Pregnancy-related deaths are defined as deaths during pregnancy and up to one year after the end of pregnancy from causes related to or worsened by pregnancy or its management. Pregnancy-related deaths, as defined in CA-PMSS, exclude deaths due to suicide, homicide, drug overdose, or other injury.
In 2018-2020, California had 1.3 million births and 208 pregnancy-related deaths. This fact sheet shares insights pregnancy-related mortality trends, including information on leading causes of death and disparities in race, ethnicity, health insurance and social determinants of health.
Key findings include:
- California’s rate of pregnancy-related deaths increased in 2020 during the COVID-19 pandemic; in 2020, there were 18.6 pregnancy-related deaths per 100,000 lives births.
- Leading causes of pregnancy-related mortality include: cardiovascular disease (CVD), hemorrhage (HEM), infection (INF), thrombotic pulmonary embolism (TPE), amniotic fluid embolism (AFE), and hypertensive disorders of pregnancy (HDP). There was a 45% decrease in pregnancy-related deaths from hypertensive disorders.
- Racial and ethnic disparities in pregnancy-related deaths decreased in 2018-2020 but persist. The rate for Black birthing people was 45.8 deaths per 100,000 live births in 2018-2020, which is 3.1 to 3.6 times higher than the rates for Asian (15.0), Hispanic/Latino (14.8), and White birthing people (12.6). In 2015-2017, the rate of pregnancy-related deaths for Black birthing people was 4.5 to 6.0 times higher.
- The disparity in the rate of pregnancy-related deaths for birthing people with Medi-Cal health coverage and those with private health insurance widened in 2018-2020. The rate for birthing people with Medi-Cal health coverage was 21.5 deaths pern 100,000 live births in 2018-2020; 2.7 times higher than the rate of 7.8 deaths per 100,000 live births for birthing people with private insurance. In 2015-2017, the rate of pregnancy-related deaths was 1.7 times higher for birthing people with Medi-Cal health coverage.
- Disparities in the rate of pregnancy-related deaths persisted based on community conditions. The rate for birthing people living in the least healthy community conditions was 18.9 deaths per 100,000 live births in 2018–2020; 2.1 times higher than the rate of 9.2 deaths per 100,000 live births for birthing people living in the healthiest communities. In 2015–2017, the rate of pregnancy-related deaths was 1.7 times higher for birthing people living in the least healthy communities. Community conditions were measured using PHI’s Healthy Places Index.

Our role in aggregating the stories of young birthing people lost too soon is important to show trends in causes of death over time, identify demographic disparities and examine the larger community context and structural factors that may be contributing to these tragic events.Christy McCain, MPH
Research Scientist
“Despite a rise in pregnancy-related mortality rates due to the COVID-19 pandemic in 2020, deaths due to hypertensive disorders of pregnancy (e.g., preeclampsia/eclampsia) declined significantly. This may be a result of the Hypertensive Disorders of Pregnancy toolkit that was developed based on findings from the CA Pregnancy-Associated Mortality Review,” said PHI’s Christy McCain, MPH, CA-PMSS research scientist. “In addition, we used findings from the Healthy Places Index (a PHI-sponsored project) to examine patterns of mortality based on larger social determinants of health versus only looking at individual characteristics.”
“PHI is proud to continue to be a part of this collaborative effort,” added McCain. “Our role in aggregating the stories of young birthing people lost too soon is important to show trends in causes of death over time, identify demographic disparities and examine the larger community context and structural factors that may be contributing to these tragic events.”
Funded by the federal Title V Maternal and Child Health Block Grant, CA-PMSS relies on a collaboration with three key partners: The Public Health Institute, Stanford University’s California Maternal Quality Care Collaborative and a volunteer review committee of experts. Learn more.
Originally published by California Department of Public Health
Work With Us
You change the world. We do the rest. Explore fiscal sponsorship at PHI.
Support Us
Together, we can accelerate our response to public health’s most critical issues.
Find Employment
Begin your career at the Public Health Institute.


